31 October 2024
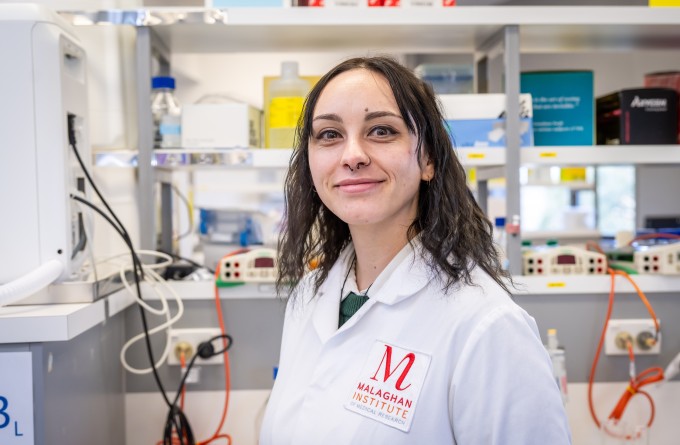
PhD student Hannah Boswell is developing vaccines that can be inhaled, providing localised immunity in the lungs and airways and stopping respiratory viruses at the very point they enter the body.
It’s time for your annual flu shot. You receive the small package you ordered in the post. You open it and find a small container with a nozzle. You tilt your head back, insert the nozzle into your nostril and press it firmly as you inhale deeply. You feel the odd sensation of mist shooting up your nose, but it swiftly subsides. You throw the container in the bin. That’s it, you’re protected against the most recent strain of the influenza virus. You carry on with the rest of your day without giving it another thought.
“We may have a few steps to take before we’re there, but we’re on the path. This could be the future of vaccines, think about how easy it would be to deliver and administer. We could protect more of our population against some of the most harmful infectious diseases,” says Hannah, who is undertaking her PhD at the Hermans Laboratory at the Malaghan Institute and the Connor Laboratory at Te Herenga Waka – Victoria University of Wellington.
“I’m working on developing an effective nasal vaccine against viruses that infect our respiratory system. We’re hoping these vaccines will induce a very specific, potent immune response within the cells of our airways and lungs,” says Hannah.
“The lungs’ immune system is unique. As an organ that constantly interacts with the air we breathe, it houses specialised immune cells that provide ongoing protection from environmental threats.”
Two key immune cells in the lungs are mucosal associated invariant T (MAIT) cells and natural killer (NK) T-cells. These cells reside in the lungs and play a crucial role in defending the body. Each type of cell is activated by specific molecules and has distinct immune functions.
“Molecules that specifically activate MAIT and NK T-cells in the lungs have been identified,” she says. “Now, we’re studying how these cells communicate with other immune cells and whether their activation can trigger a safe, long-lasting immune response in a vaccine.”
“Ideally, this could result in sterilising immunity, meaning the vaccinated person would be unable to transmit the virus to others.”
The focus of Hannah’s research is to determine if stimulating MAIT and NK T-cells with these molecules can create a sustained protective response, potentially making the molecules effective adjuvants for nasal vaccines.
“All vaccines have two main components,” says Hannah.
“The first provides the immune system with a copy of the component of the virus you want to target; this could be a whole inactivated version of the virus itself, a protein fragment of the virus, or an mRNA molecule that instructs cells to make a protein from a virus. The second is the immune adjuvant, a compound that boosts the immune system’s response. Without it, the immune system might not recognise the viral target, preventing long-term immunity.”
Adjuvants are like a courier who requires a signature for a package. They ensure the right part of the immune system receives and responds to the vaccine, rather than leaving it unattended where it could be ignored or lost.
While her current work is focused on influenza vaccines, Hannah hopes that once the mechanisms of MAIT and NK T-cells are better understood, the molecules that activate them could be used as adjuvants for nasal vaccines against other respiratory viruses, such as SARS-CoV-2 and RSV.
“The advantage of a nasal vaccine that activates immune cells in the lungs and airways is that it provides protection where respiratory viruses first enter the body. This allows the immune response to act immediately, reducing the likelihood of the infection taking hold,” says Hannah.
“Ideally, this could result in sterilising immunity, meaning the vaccinated person would be unable to transmit the virus to others.”
Nasal vaccines would be particularly valuable during a pandemic, where limiting physical contact is crucial for controlling the spread of infection. If the vaccine could be delivered by post and self-administered, it would reduce the strain on healthcare workers, allowing them to focus on critical care.
“Having found my niche in immunology, I’d say it’s the perfect combination of nitty gritty detail with the potential for significant human impact.”
Hannah loves diving into the nuts and bolts of her research to understand how intricate details apply to the whole system. However, this interest in the fundamentals is not where her career aspirations initially lay.
“Until I was about 16, I wanted to be a zookeeper. I don’t quite know where that dream came from but in the last years of high school it evolved into a general love of biology.”
“I decided I wanted to be a doctor but quickly decided against it as soon as I started my undergraduate in biomedical science at the University of Otago. I was interested in more of the intricacies of cells and less in monitoring physiological symptoms and clinical matters.”
Hannah studied MAIT cells for her BSc honours project, investigating how they interact with other immune cells.
“My PhD research has enabled me to expand on my knowledge on MAIT cells and explore other immune cell types like NK T-cells to understand how they help induce a protective immune response,” says Hannah.
“Having found my niche in immunology, I’d say it’s the perfect combination of nitty gritty detail with the potential for significant human impact.”
Related articles
How our immune system tackles fungal foes
23 October 2025
New funding supports cutting-edge research into immune cell metabolism
13 October 2025
The Detail: The viral drift of misinformation
29 September 2025

Blood, sweat and cells: The making of New Zealand’s first CAR T-cell trial
24 September 2025

Cancer, measles and allergic disease research funded in latest HRC grants round
19 August 2025
Dr Lisa Connor: Finding new ways to target old viruses
24 July 2025
