12 July 2022
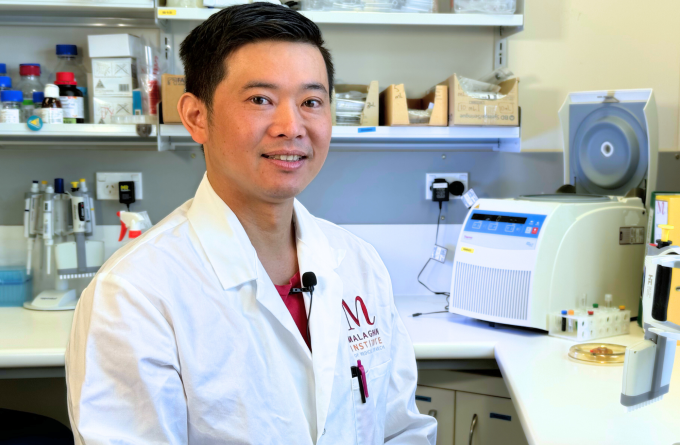
With his background in structural biology and virology, Dr Jordan Minnell is tailoring mRNA vaccines to activate immune cells in the liver to target diseases such as malaria and hepatitis B.
Dr Jordan Minnell is one of the many scientists around the world whose current field of research was an obscure yet hopeful vision for the future before the COVID-19 pandemic. Over the last few years, RNA technology has taken off, playing an essential role in our ability to produce effective vaccines in record-breaking time. Today Jordan is working on developing mRNA vaccines to induce protective immunity in the liver against pathogens that target the liver.
There are specialised immune cells in our different organs called tissue resident memory T-cells. These cells are like the special forces for each organ who have been warned of a specific threat that might breach their territory. They lie in wait, clutching the wanted poster with the likeness of the invader, ready to raise the alarm to call in reinforcements before they unleash a deadly assault.
Jordan is working to create more of these special forces in the liver so they can be better prepared for specific invaders.
“The overall goal is to get a lot of memory T-cells into the liver by administering an intramuscular vaccine,” says Jordan. “We’re engineering and tinkering with the mRNA vaccine components to see which combinations produce the best immune response.”
mRNA vaccines are composed of two fundamental components: the RNA molecule which is like the wanted poster, and a lipid nanoparticle which encapsulates the wanted poster like an envelope and delivers it to the right location. Creating an effective mRNA vaccine means tweaking and testing these components to most effectively stimulate the immune response. Jordan is also looking to add additional components called adjuvants to increase this response.
“We've got a collaboration with the Ferrier Research Institute where we've identified some novel chemical compounds which drive the generation of tissue resident memory T-cells in the liver,” says Jordan. “Once we have an optimal vaccine model that can stimulate these memory T-cells, we can code in what pathogens these T-cells should be on the lookout for.”
Several infectious diseases target the liver. An example is malaria which has a severe impact globally: in 2020 alone, there were an estimated 241 million cases and 627 thousand deaths. Currently, there is only one approved vaccine for malaria which has limited efficacy and requires a complex regimen of doses. Jordan’s work has the potential to make a better vaccine for malaria which recruits tissue resident T-cells that will attack the parasite that causes malaria infection before it takes root.
Long before being the Malaghan Institute’s resident expert on RNA technology, Jordan did his undergraduate degree in biochemistry at the University of Otago before reaching a crossroads in his life.
“I was uncertain on whether I should be an academic or not. I nearly moved up to Wellington to hang out with my friends and become a bartender, which would have been fun,” says Jordan. “But I ran into Dr Monica Gerth who had just moved to Otago to join the biochemistry department. She offered me a place as a summer student in her lab and the rest is history.”
Jordan went on to do his Master’s degree at Dr Gerth’s lab, working in structural biology. Here, he used a technique called crystallography to uncover protein structures.
“Dr Gerth provided me with ample opportunity to prove myself and introduced me to this whole realm of academic research. She ultimately drove me to publish my Master’s research,” says Jordan.
This gave Jordan the opportunity to go to the United Kingdom and work at Imperial College London at Dr Goedele Maerten’s lab which specialised in both structural biology and virology.
Starting as a research officer, Jordan went on to do his PhD and then a postdoc working on defining the 3D structure of the point of binding between delta retroviruses and the proteins they bind to within their hosts during infection. Types of delta retroviruses include human T-cell leukaemia virus type 1 which has been linked to the development of untreatable leukaemia in an estimated 5% of those who contract the virus.
By clarifying the unique interaction between molecules at the point of virus binding, Jordan’s research has paved way for the development of potential therapies that can disrupt this binding and terminate viral infection.
In early 2021, Jordan came back to New Zealand to work in Professor Ian Hermans’ lab at the Malaghan Institute where he applies his broadly molecular skill-set to advance RNA vaccine technology.
“RNA technology has so much potential,” says Jordan. “For New Zealand to have its own R&D in this area means we are less dependent on other countries to develop vaccines and for their supply to trickle down to us. This capability will give us some agency to respond to future emerging viruses, including future variants of SARS-CoV-2,” says Jordan.
“I've got the bug, I'm really interested in learning more about where this technology can take us and using the skills that I've got to develop useful medical therapies. New Zealand has the potential to be a leader this field and I’m excited to be a part of that.”
Related articles
Fighting allergic skin disease at its root
17 December 2024
As easy as breathing: the future of vaccines
31 October 2024
As easy as breathing: the future of vaccines
31 October 2024
Fast Start grant to explore and establish next generation RNA technology
7 October 2024
CAR T-cell therapy, the battle of the blood cells
26 September 2024

Malaghan RNA researcher named KiwiNet Emerging Innovator
4 September 2024
