29 November 2021

Until recently, developing a vaccine was a time-consuming and costly process, involving the production of inactivated or weakened virus or viral proteins. It required a lot of trial and error to make these ‘artificial’ proteins look as close to the real thing as possible – a process scientists would have to repeat each time a virus mutates and changes its structure.
mRNA technology circumvents this iterative process and instead use our own cells to make the vaccine.
The process works so well because our cells already have all the machinery they need to build perfect copies of proteins. All we need to supply is the instructions. Because these instructions only code for a small part of a virus, there’s zero chance that our cells will accidentally make the real thing.
Nestled in the nucleus, at the centre of our cells, is our DNA. It contains the instructions to produce most of the building blocks, or proteins, that make up our body.
However, DNA never ventures out of its position within the fortified nucleus. Instead, it sends out a tiny messenger molecules – mRNA – which contain only the relevant instructions for our cells to make particular proteins. This intermediate messenger is required because the machinery for making proteins lives outside the nucleus. Once the information in the mRNA is read by the cell and made into a protein, it’s no longer needed and breaks down.
Because viruses are also made of proteins, by presenting the body with an mRNA molecule encoding a portion of the virus, like a spike on its surface, we can get a cell to produce copies of this protein, which then get picked up by our immune cells that can now begin the process of recognising and generating immunity.
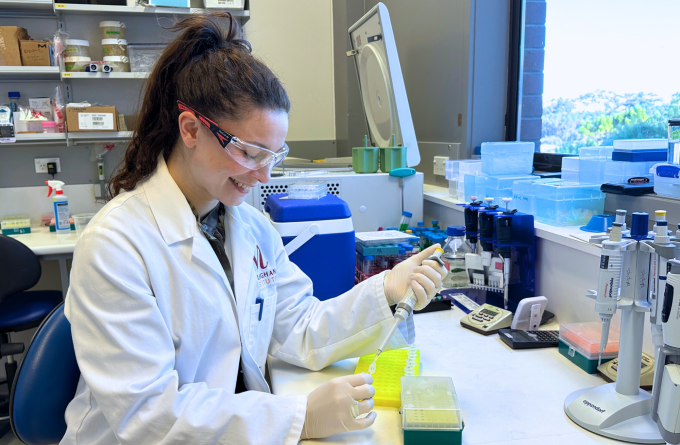
To make a new vaccine, all we need is to know the genetic code of the virus, a process that takes only a few hours. Once we know the code we can determine which bits will work best for a vaccine and generate a matching mRNA sequence. All up, it takes only a couple of days and very few resources to have a brand new vaccine, compared to sometimes years using the traditional method. Once it’s gone through the safety testing, billions of doses can be made and distributed from a single lab.
Related articles

Malaghan RNA researcher named KiwiNet Emerging Innovator
4 September 2024
In Focus: Fever, too hot to handle or the body's first line of defence?
22 August 2024

In Focus: Rejuvenating the ageing immune system
17 July 2024
Hugh Green Technology Centre: driving innovation and support of medical research
12 July 2024

Kia Niwha Leader Fellowship for Malaghan vaccine researcher
6 May 2024
In Focus: Mapping the lung's fight – how the entire organ responds to infection
18 April 2024
