17 July 2024
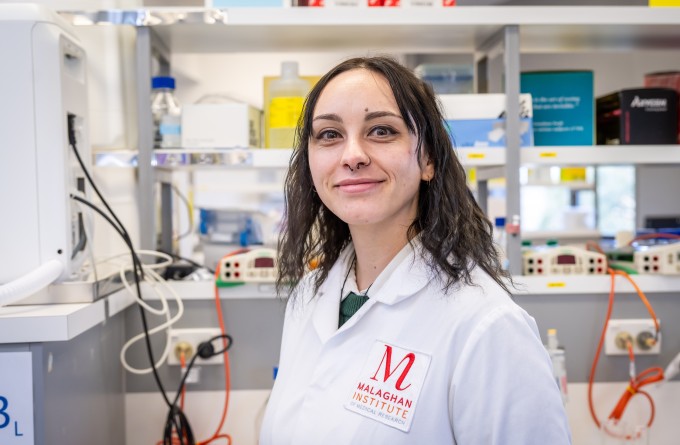
The body’s ability to overcome infection becomes less effective as we age. In an international research effort, Dr Theresa Pankhurst is focused on producing vaccines to revitalise the ageing immune system.
During the Covid-19 pandemic, more than 74% of global deaths occurred in people over the age of 65. Likewise, most deaths from respiratory viruses like influenza and RSV occur in people in this older age group, with risk increasing sharply with advancing age. So, what happens as we age that reduces our body’s ability to fight infections? And what can we do to power up the immune system in later stages of life? These are questions that Malaghan postdoctoral research fellow Dr Theresa Pankhurst is trying to answer.
Theresa (Ngāi Tahu, Ngāti Kahungunu, Ngāti Porou) is undertaking research in fellow Kiwi Dr Michelle Linterman’s lab at the Babraham Institute in Cambridge, UK. Theresa has been awarded both the Te Urungi Churchill College Fellowship and Te Niwha’s Kia Niwha Leader Fellowship to support her research to develop vaccines for the ageing immune system, a collaboration between the Babraham and Malaghan Institutes.
“My project at the Linterman lab focuses on how our immune system changes as we age, and what the implications are for the protective immunity provided by vaccines,” says Theresa.
“We then design vaccines that aim rejuvenate a part of the immune system that becomes less effective in later life using the Malaghan Institute’s RNA platform.”
“We’re especially interested in germinal centres, temporary structures that form in our lymph nodes after infection and vaccination to produce antibody secreting cells that can provide protection against future infections.”
Germinal centres are a part of the immune system that do not function as well as we age and the part of the immune system that Theresa’s research aims to reinvigorate.
While we get on with our lives, our bodies are on continuous alert for infectious agents that might threaten the carefully maintained balance within us. When an infectious agent such as an influenza virus enters the body, it multiplies. As the infection progresses, the virus leaves behind fragments that give away its presence. These fragments are picked up by immune cells patrolling our bodies whose role is to detect any foreign intruders that might pose a threat.
“To create a germinal centre, the cells of the immune system must get together at the right place, and at the right time. Of these, two types of immune cells, a B-cell and a T follicular helper cell must identify the same part of a pathogen to be a threat,” says Theresa.
“These two cells then convene and exchange this information as confirmation that this is indeed a threat so as to minimise the chance of an immune attack being launched against the body’s own cells.”
This safety mechanism is like a nuclear launch where two keys must be inserted by two highly ranked military personnel as a precautionary measure. Instead of missiles, this signal initiates the steps to set up a germinal centre: a highly specialised weapons factory. Germinal centres produce powerful B-cells capable of launching antibodies that target and neutralise the detected threat.
“We are developing mRNA vaccines that rejuvenate this powerful immune process in older people.”
A germinal centre is highly organised, split into the dark zone and the light zone. In the dark zone, the B-cells are manufactured, each with slightly different binding sites. These new B-cells advance to the light zone where each is tested and judged according to its ability to target the threat.
An important cell in this process is the T follicular helper cell which waits in the light zone, acting as the examiner and giving each B-cell a pass or fail according to whether it is activated by a fragment of the infectious agent.
If the B-cell is activated by the fragment, it passes the test, and the T follicular helper cell gives it a signal that ensures the B-cell’s survival. If the B-cell is not activated by the fragment, the T follicular helper cell gives no signal and the B-cell dies.
Of the B-cells that survive, they are destined for one of three fates. They can be sent back into the dark zone for further refinement, or exit the germinal centre as a plasma B cell or a memory B cell.
Plasma B-cells trigger a powerful assault, releasing antibodies that neutralise the threat, tagging it to be engulfed by other immune cells. Memory B-cells, on the other hand, lie dormant in the bone marrow like reserve weapons waiting for future activation.
“This is a truly fascinating process of microevolution within our own bodies where the cells that are able to respond to a specific threat are selected to survive,” says Theresa.
“Each B-cell is slightly different. This is to maximise the chances of recognising future variants of the infectious disease which will be slightly different to the current infectious agent.”
Once the specialised plasma and memory B-cells are produced and the body no longer recognises the presence of infection, the germinal centre, having served its purpose, is dismantled.
The activity of the germinal centre provides us with a powerful defence against infectious diseases. This mechanism also activates during vaccination which produces B-cells, ready for an immediate attack in the event of an actual infection.
However, as we age, this process becomes less effective meaning fewer antibodies are produced in response to infections and vaccinations.
“Recently, the Linterman lab published a seminal study which found that the T follicular helper cells, which give the survival signal to effective B-cells, meander to the dark zone rather than remaining in the light zone to carry out their pivotal function,” says Theresa.
“We are developing mRNA vaccines that rejuvenate this powerful immune process in older people, and one method we are investigating is stimulating T follicular helper cells.”
These vaccines are designed at the Babraham Institute, synthesised and optimised at the Malaghan Institute, then sent to the Babraham Institute to be tested by Theresa on specialised animal models.
“I have limited time from when these mRNA vaccines arrive at the Babraham Institute and are viable to be tested. I just have to hope the post arrives on time!”
“The vaccines are being tested in younger adult and aged mice. Their protective capacity is assessed after influenza virus infection by measuring if they can prevent lung disease,” Theresa says.
“In the future, I can return to Aotearoa New Zealand and use what I have learned to help create solutions to problems that afflict vulnerable populations in our community.”
This project illustrates the international nature of scientific research, a vast network of people, knowledge and resources that feed into each other to provide solutions to our most pressing issues.
“Despite being an isolated set of islands in the Pacific Ocean, Aotearoa New Zealand can make significant contributions to the global scientific field. To do this well, we need to establish and maintain international collaborations, so we stay up to date with the blistering pace of global scientific research.”
Theresa spent her early years in Invercargill before her family moved to Christchurch where she attended St Andrew’s College. Theresa then completed a biomedical science degree at Te Herenga Waka – Victoria University of Wellington, coincidentally, the same university and degree as Dr Michelle Linterman who went on to an international research career in Australia and then Cambridge for the last fifteen years.
Theresa did her Master’s before undertaking her PhD with Te Herenga Waka and the Malaghan Institute, focusing on creating mucosal vaccines for infectious viruses such as influenza and SARS-CoV-2. Following her PhD, she worked at the Malaghan Institute before embarking on her adventure to Cambridge.
“I am doing this fellowship here at the Babraham Institute to learn new scientific techniques, make connections and get new perspectives so that in the future, I can return to Aotearoa New Zealand and use what I have learned to help create solutions to problems that afflict vulnerable populations in our community.
I am incredibly grateful to the Malaghan Institute’s Te Urungi Māori and Te Niwha for the opportunity to conduct this research and build leadership skills to make my future goals a reality.”
Related articles

How a quirk of the immune system may play a big role in protecting us from disease
18 December 2025

The nose knows: new research explores next generation of nasal vaccines
2 December 2025

Tracking the journey of the shapeshifting bacteria behind stomach cancer
19 November 2025

Marsden funding to drive discovery and innovation in cancer, allergy and infectious disease research
5 November 2025
How our immune system tackles fungal foes
23 October 2025
New funding supports cutting-edge research into immune cell metabolism
13 October 2025
