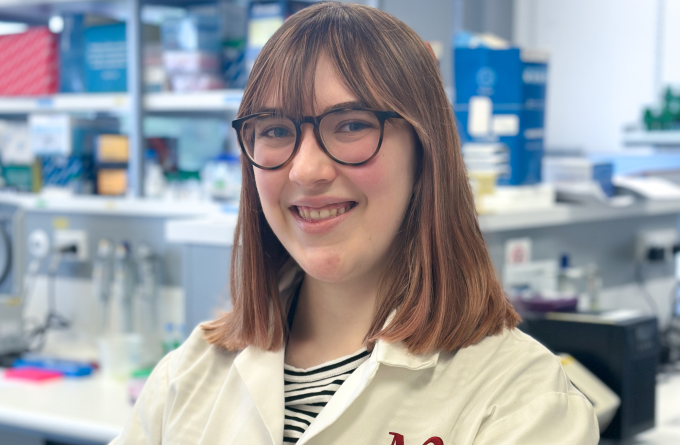
Dr Lisa Connor
Programme Leader - Connor Laboratory
PhD (Otago) BMedSc(Hons) (VUW)
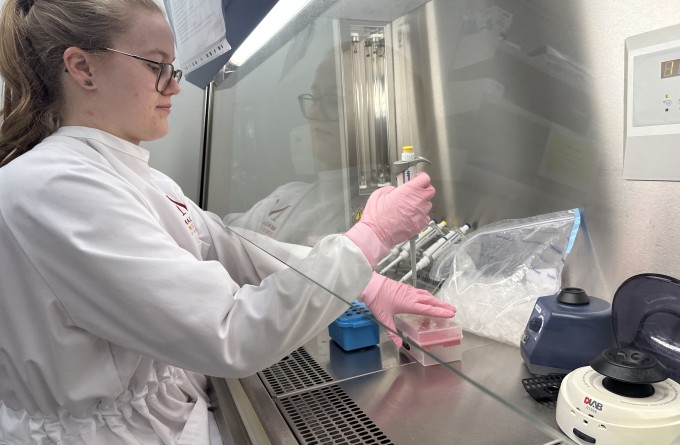
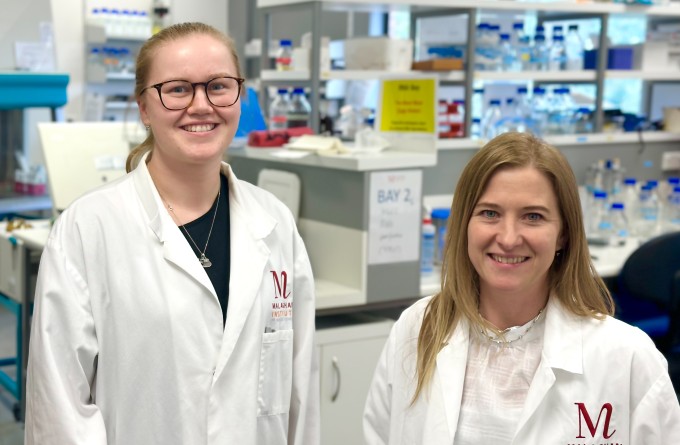
Dr Lisa Connor is the head of the Connor Laboratory and Programme Leader of the Infection and Vaccinology Group at the Malaghan Institute. Her research focuses on the immunobiology of vaccination, aiming to build better vaccines by understanding fundamental mechanisms of immune activation. Dr Connor's work explores dendritic cell activation post-immunisation, the necessity of T follicular helper cell activity, and its impact on B-cell responses and antibody production.
Specialising in combating respiratory viruses, the Connor Laboratory develops mucosal vaccines and harnesses mRNA vaccine technology to design smarter antigens. Dr Connor has played a pivotal role in enhancing Aotearoa’s vaccine development capabilities, leading a COVID-19 vaccine programme and serving as preclinical pillar lead for the New Zealand RNA platform.
Dr Connor completed her PhD at the Malaghan Institute and the University of Otago, under the supervision of A/Prof Joanna Kirman, where she investigated CD4 memory T-cell responses to BCG vaccination. She then pursued postdoctoral research at the Trudeau Institute in Upstate New York with Dr David Woodland, studying memory CD8 T-cell responses to respiratory viruses. Returning to Aotearoa, Dr Connor focused on deciphering the biology and transcriptional profile of dendritic cells with Professor Franca Ronchese and was awarded the prestigious Sir Charles Hercus Research Fellowship in 2018.
Dr Connor established her laboratory in the School of Biological Sciences at Te Herenga Waka—Victoria University of Wellington in 2018 and in January 2025, she took up her current position at the Malaghan Institute.
Related news
As easy as breathing: the future of vaccines
31 October 2024
Malaghan scientists appointed in leadership roles in New Zealand's RNA Platform
31 May 2024
In Focus: Tailoring mRNA vaccines for immunocompromised populations
14 December 2023
Stopping infections at the door – designing vaccines that target immune cells in the mucosa
19 April 2023

Kiwi-made Covid-19 booster vaccine offers 100% protection in preclinical study
3 March 2023
Homegrown COVID-19 booster vaccine: building New Zealand’s biomedical capability
23 May 2022
Publications
2024
Pankhurst TE, Montgomerie I, Marshall A, Draper SL, Bilbrough T, Button KR, Palmer OR, Hermans IF, Painter GF, Connor LM, Compton BJ (2024). A Glycolipid-Peptide-Hapten Tricomponent Conjugate Vaccine Generates Durable Antihapten Antibody Responses in Mice. ACS Chem Biol. 19(6):1366-1375
2023
Pankhurst TE, Buick KH, Lange JL, Marshall AJ, Button KR, Palmer OR, Farrand KJ, Montgomerie I, Bird TW, Mason NC, Kuang J, Compton BJ, Comoletti D, Salio M, Cerundolo V, Quiñones-Mateu ME, Painter GF, Hermans IF, Connor LM (2023). MAIT cells activate dendritic cells to promote TFH cell differentiation and induce humoral immunity. Cell Rep. 42(4):112310
Montgomerie I, Bird TW, Palmer OR, Mason NC, Pankhurst TE, Lawley B, Hernández LC, Harfoot R, Authier-Hall A, Anderson DE, Hilligan KL, Buick KH, Mbenza NM, Mittelstädt G, Maxwell S, Sinha S, Kuang J, Subbarao K, Parker EJ, Sher A, Hermans IF, Ussher JE, Quiñones-Mateu ME, Comoletti D, Connor LM; On behalf theVAANZ Group (2023). Incorporation of SARS-CoV-2 spike NTD to RBD Protein Vaccine Improves Immunity Against Viral Variants. iScience. 26(4):106256
2021
Mayer JU, Hilligan KL, Chandler JS, Eccles DA, Old SI, Domingues RG, Yang J, Webb GR, Munoz-Erazo L, Hyde EJ, Wakelin KA, Tang SC, Chappell SC, von Daake S, Brombacher F, Mackay CR, Sher A, Tussiwand R, Connor LM, Gallego-Ortega D, Jankovic D, Le Gros G, Hepworth MR, Lamiable O, Ronchese F (2021). Homeostatic IL-13 in healthy skin directs dendritic cell differentiation to promote TH2 and inhibit TH17 cell polarization. Nat Immunol. 2021 Nov 18
