22 August 2024
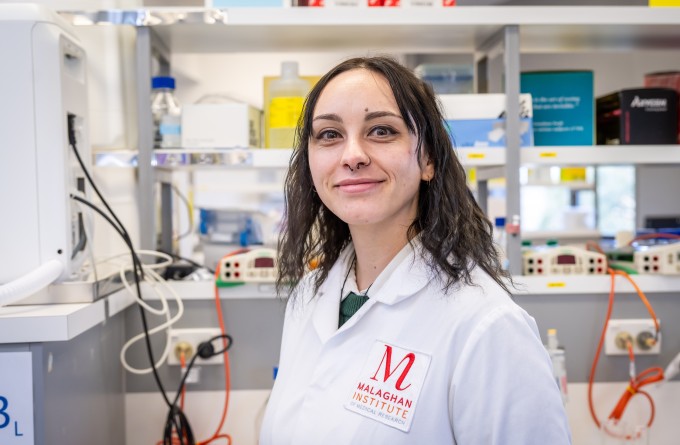
Malaghan PhD student Rosemary Jackson is investigating the effect of fever on our immune system. By taking a deep-dive into T-cell activity, her work is challenging whether our current approach to managing fever is the best way to overcome infectious disease.
Rosemary remembers one of the worst experiences of her life. Every inch of her body was aching, she was both delirious and nauseous. The arid, sub-Saharan air stoked the scorching heat of her body. She was lying facedown on a mercifully cool slab of concrete, pleading for the heat and pain to leave her body.
Rosemary had contracted malaria. To make things worse, she had minimal access to medical care, her only relief from the sustained fever and pain coming from paracetamol and ibuprofen.
She has come a long way from her time in South Sudan in her early twenties. Rosemary is now back in New Zealand where she is undertaking her PhD in the Gasser Laboratory at the Malaghan Institute, supervised by Dr David O’Sullivan.
“Fever happens when our immune system detects a threat and communicates the presence of an infection to our brains. Our body’s thermostat, located in part of our brain called the hypothalamus, then turns up the heat,” says Rosemary.
Our body’s average temperature is about 37oC. This increases to 38oC for a low-grade fever and up to 41oC for a high-grade fever. Maintaining this higher temperature takes a huge amount of energy and is very taxing on the body.
“As most of us have experienced, this feels miserable. Fever can bring about crippling fatigue that leaves you unable to carry out your daily functions, along with body aches and loss of appetite,” says Rosemary. “Paradoxically fever also makes us feel like we’re cold – making us seek the warmth of blankets and heaters.”
This physiological response is common across all mammals. Even cold-blooded animals such as fish and reptiles will seek out warmth during infections to raise their body temperature. This indicates that a higher temperature may be beneficial to the body in some way during infection.
“Everyone has heard grandma’s advice to ‘let the fever run its course’, that an increased body temperatures will drive out whatever is infecting the body,” says Rosemary.
“What if that wasn’t entirely unhelpful advice? In our modern lives, we tend to run away from any uncomfortable experience. We tend to think of fever as being a product of the infection rather than our body’s own way of launching an attack against the infection.”
“We’re hoping that this research will help us to find a more nuanced approach to managing fevers.”
Fevers can create a hostile environment and inhibit the growth of infectious agents such as invading bacteria and viruses which are adapted to normal human body temperature.
“What is less known is how fevers also serve to aid our body’s offensive strategy against the infectious agent. Some evidence suggests the increased temperature results in enhanced immune function, helping white blood cells, including T-cells, kick into gear to overcome the infection.
Rosemary’s research is investigating if a mild to moderate fever helps T-cells mount a stronger attack against infections. Specifically, she is looking into how T-cells change on a molecular level during increased temperatures and how long the fever needs to be sustained to bring about any beneficial changes in the T-cells.
“T-cells are some of our most important immune cells. Part of their response involves a rapid expansion phase where one highly specialised T-cell will become activated and multiply to produce a whole army of clones that can target and kill the specific threat.
“For this rapid expansion of immune cells to occur, the body needs an increase in both energy and building materials for those new cells. It’s possible that elevated temperatures help the T-cells to do this more effectively, ‘supercharging’ them from the inside.”
Rosemary is conducting experiments taking T-cells and then activating them at either normal temperature (37oC) or moderate fever temperature (39oC) and leaving them overnight. This mimics common patterns where an individual gets sick in the evening and has a fever overnight which then subsides in the morning.
She then monitors the cellular and molecular changes that occur over the next several days in both these sets of T-cells to understand if there is any difference in the cells which were activated at fever temperatures.
“So far, we’ve found some very interesting results. T-cells that were exposed to fever-like temperatures for several hours when activated, along with their subsequent generations of clones, showed increased immune activity even several days after being returned to normal body temperature.”
“In contrast, T-cells kept at normal body temperature from the start did not show this same heightened activity. This suggests that even a brief period of increased temperature triggered signals within the cells that were passed down to their clones, instructing those clones to become more potent in their immune response.”
She will soon begin studying these effects in infectious disease models including influenza, to see how these molecular changes in T-cells may alter the immune response during infection.
“We’re hoping that this research will help us to find a more nuanced approach to managing fevers. Rather than having a blanket approach where fever-supressing medicines are used in all cases, perhaps it would be more beneficial to carefully monitor the fever, and let the fever run its course within a reasonable time and temperature window.”
“It’s very important to listen to medical advice from healthcare professionals as sustained, or very hot fevers can be dangerous.”
Thinking back to her experience with malaria, Rosemary acknowledges that sometimes fever can be unbearable and damaging to the body so it’s better to reach out for relief in the form of modern medicine.
“It’s very important to listen to medical advice from healthcare professionals as sustained, or very hot fevers can be dangerous,” stresses Rosemary.
Contracting malaria was a unique start to biomedical sciences for Rosemary. After completing high school in Gisborne, she sought adventure and enrolled in a degree in cultural anthropology at Te Herenga Waka – Victoria University of Wellington. However, she quickly realised it wasn’t the right path for her and instead headed overseas, volunteering at a children's home in Yei, South Sudan. However, after a few months, she unexpectedly found herself in the middle of a civil war, caring for 130 children. With mass evacuations underway, medical care in the city became almost non-existent, and basics like food and fuel became scarce. Rosemary was forced to step in, dressing wounds and treating infections on a daily basis, under the supervision of two American nurses. During her 18 months there, she contracted malaria three times.
“I don’t think I really knew what I was getting myself into. I was so naively optimistic, I wanted to make a real difference in the world. I don’t think I could do what I did then now, but I learned so much from the experience,” reflects Rosemary.
After returning to New Zealand, it took her some time to adjust. Initially, she thought medicine might be her calling, but she soon developed a deep interest in immunology. After doing her Master’s at Victoria University, she came to the Malaghan Institute in 2022 as a summer student.
“I don’t think I wanted to be a doctor after everything I’d witnessed. A quiet life behind the scenes, doing meaningful research, feels like the perfect path for me.”
Rosemary walking alongside a few of the children she was looking after in South Sudan
Related articles
How our immune system tackles fungal foes
23 October 2025
New funding supports cutting-edge research into immune cell metabolism
13 October 2025
The Detail: The viral drift of misinformation
29 September 2025

Blood, sweat and cells: The making of New Zealand’s first CAR T-cell trial
24 September 2025

Cancer, measles and allergic disease research funded in latest HRC grants round
19 August 2025
Dr Lisa Connor: Finding new ways to target old viruses
24 July 2025
